All Procedural Skill Trainers Are NOT Created Equal
Operating a simulation center using and implementing SBE (simulation-based education) tools to train future healthcare providers must balance efficient and effective training in high volume with quality training within a rapidly changing and advancing scope of technology. Investing too much capital in fixed assets will drive up costs but invest too little you risk being left behind in a dark age of technology. Not every new gimmick or tech trend is needed in order to deliver high-quality evidence-based training to healthcare professionals, you just need to find the most cost-effective method suitable to your volume of demand.
It is important for task trainers used in procedural simulation to mimic real world situations to promote safe and effective learning. Attention and care should be taken to minimize any negative learning during simulation. Therefore, it is vital that task trainers are evaluated for usability, fidelity and the ability of the simulation tool to help learners reach their objective.
Thoracostomy Simulators for Procedural Training:
Chest tube insertion is required for most cases of traumatic pneumothorax. However, this procedure entails risks of potentially life-threatening complications and a “surgical” approach is widely recommended to minimize these risks. Hospitals and third-party payers experience increased costs with surgical complications, with hospitals experiencing a reduction in profit margin. Both hospitals and payers appear to currently have financial incentives to promote surgical quality improvement.
There is a need for a low cost, low resource chest tube trainer for procedural education for multiple learner populations in healthcare and health professions programs. There are several trainers that are commercially available at a high cost and are therefore not feasible for many institutions.
Option: DIY
With 5 years of experience in the realm of procedural training using evidence based deliberate practice, I have come into contact with a wide range of procedural skills trainers and an even wider field of their individual capabilities. Some offer “capability A” but lack in “capability B” often resulting in the purchasing of additional trainers to meet simulation center needs. Workarounds are also common when certain products fall short.
A Case In Point: When offering Central Line Placement training in our Procedural Skills Lab, our Blue Phantom trainers could not withstand cutting, dilation or suturing even though manufacturer recommendations allowed for this practice. Due to the volume of learners we were aiming to train and the rate at which we would be required to replace manikin inserts, this did not make for a cost-effective best practice method for our simulation center needs. There was an integral part of the procedure that was missing from our training curriculum. A critical portion of the procedure that was key to lowering infection rates (i.e. the use of sterile precautions in securing and dressing of insertion site by clinician who performed the catheter placement).. Our workaround in this case was to create a silicone model for completing the learner’s skill set. We dubbed this, “the completion trainer”.
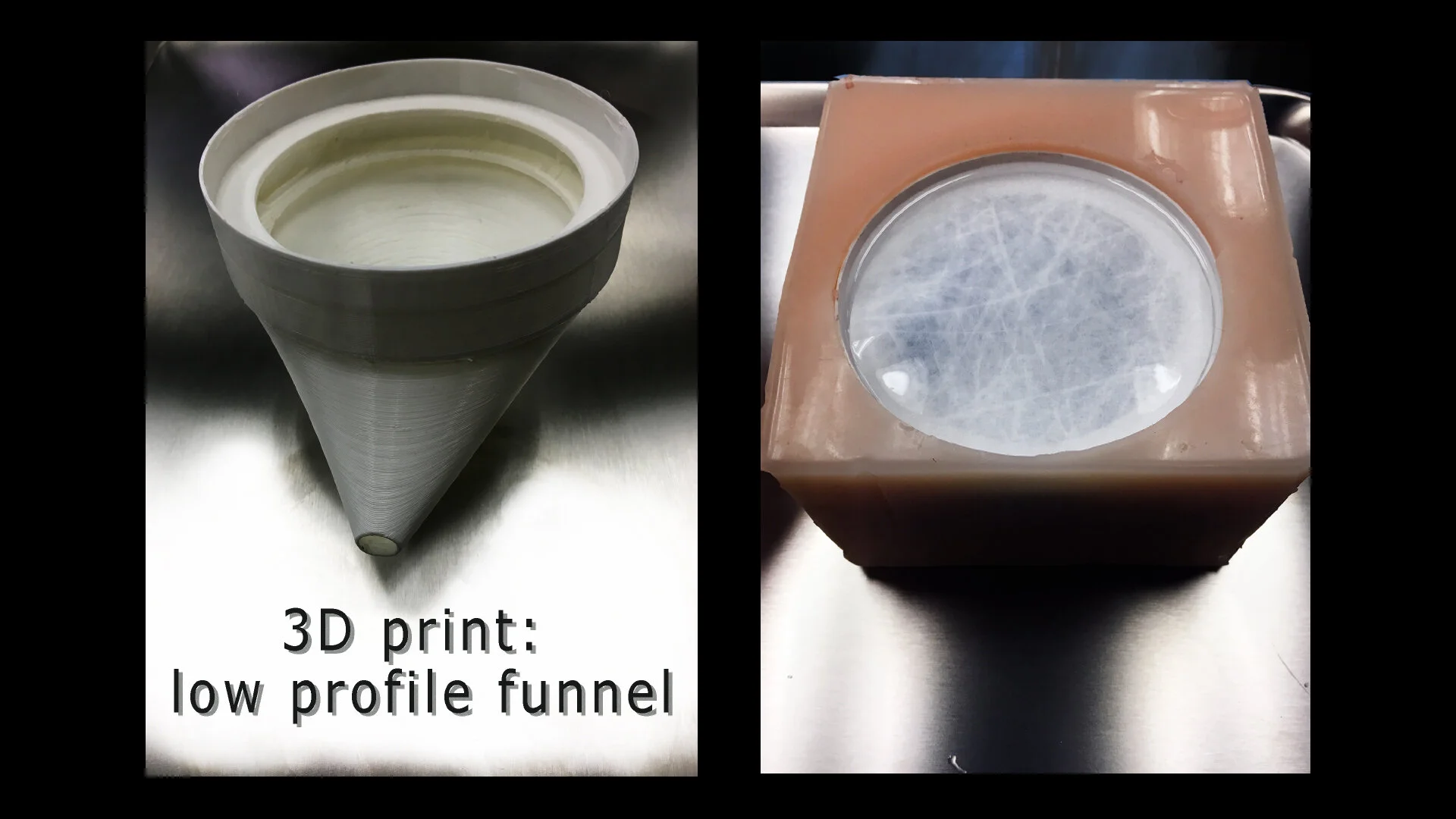
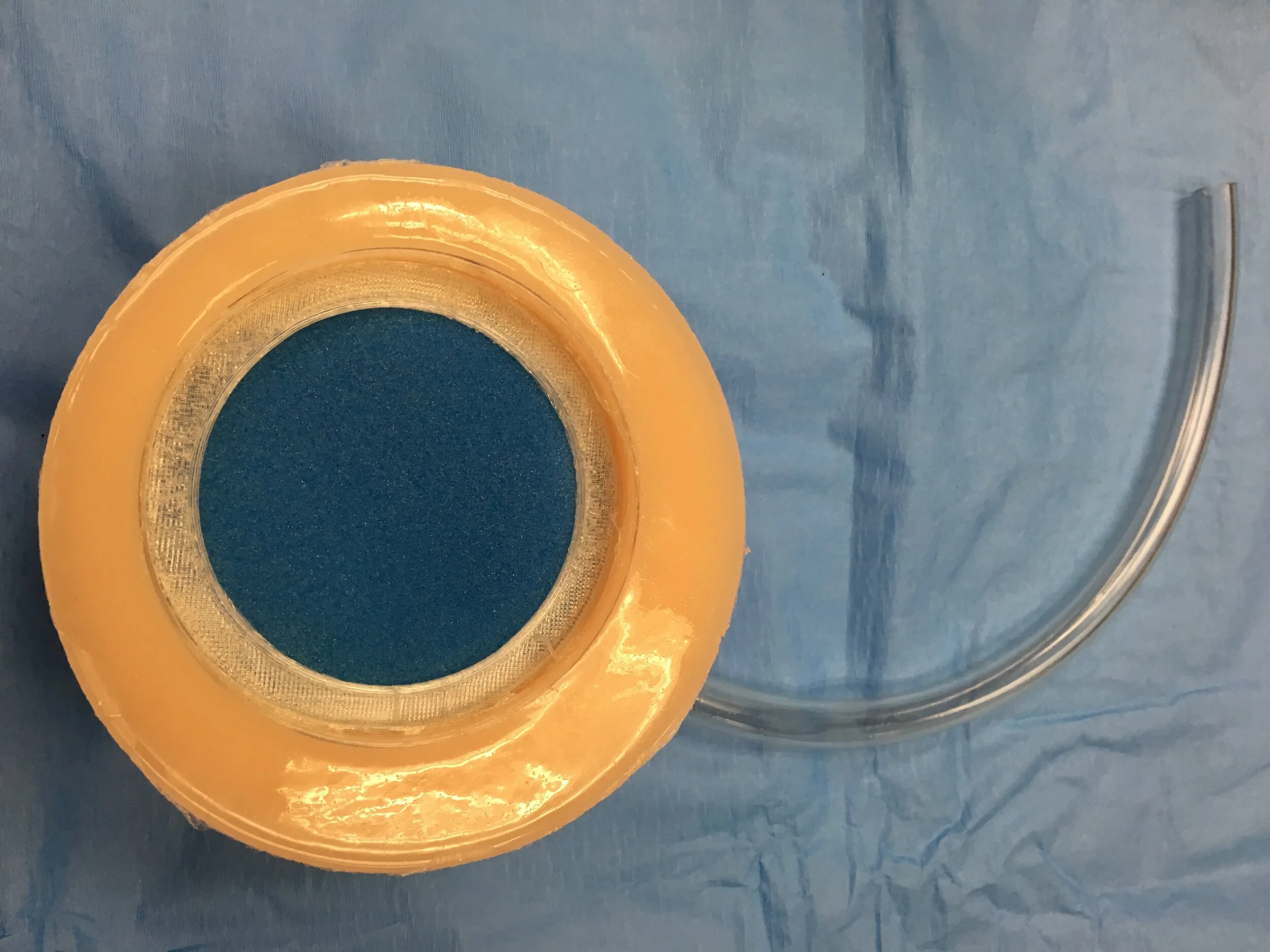
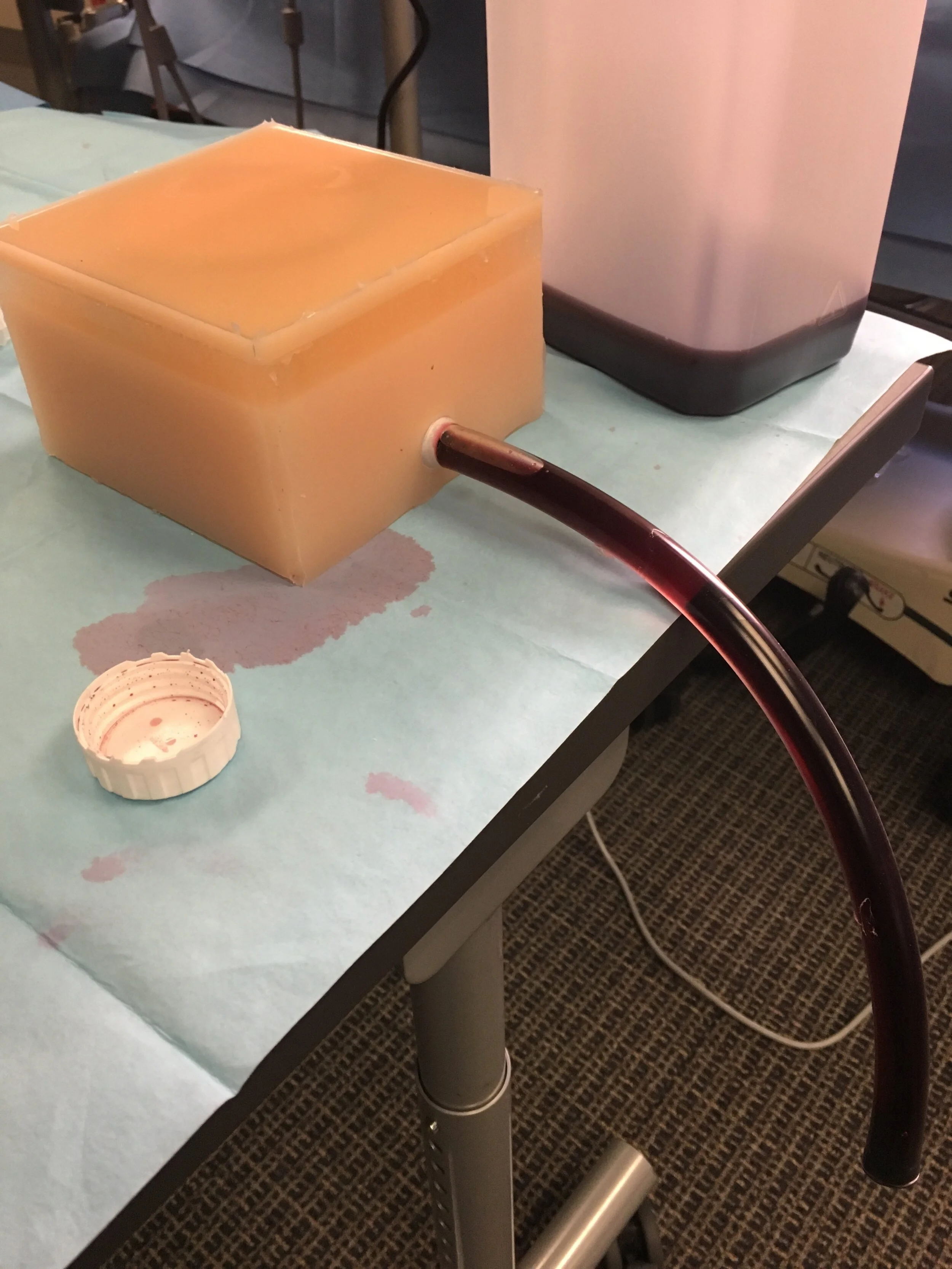
A combination of silicone, 3d printed internal funnel and a surface area suitable for dilation and securing catheters with sutures and able to be refurbished up to 10 times using a minimal amount of effort and materials. Using a similar workaround measure and lessons learned from a variety of successful and not so successful silicone based endeavors, a silicone based chest tube insertion model was created to offset the cost and effectiveness of our higher priced commercial thoracostomy trainer with which had received several negative feedback comments in the past.
A Method to Madness:
Using a readily available tutorial for a silicone injection trainer from a silicone manufacturer as the impetus, I put to use my background as a student of the visual arts and possibly the genes of a “mad scientist” for this creation. The injection trainer formula was “upsized” and modified to fit a cardboard based rib cage with varying degrees of silicone materials each meant to mimic the various human tissue encountered while performing this procedure.
After several iterations based on content expert feedback, a low-cost, low-resource thoracostomy trainer is well within our sights for implementation into standard thoracostomy training for Emergency Medicine interns as part of our procedural skills training curriculum.